August 28, 2025
4 min read
New Cell Transplant for Type 1 Diabetes Sidesteps Need for Immunosuppressants
Scientists treated a person’s type 1 diabetes with genetically modified insulin-producing cells that evaded immune system attacks. This is the first therapy for the condition that does not require immunosuppressant drugs
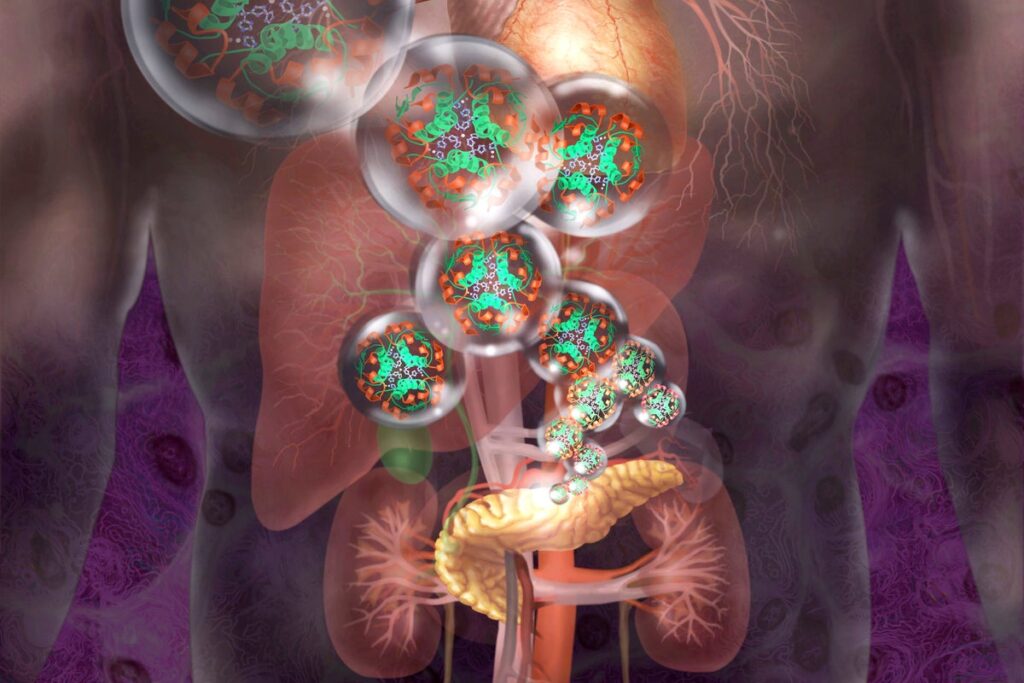
Insulin-producing cells can be genetically modified to hide from the immune system.
Jim Dowdalls/Science Source
People with type 1 diabetes must constantly rely on insulin injections or pumps, usually for the rest of their life after diagnosis. The autoimmune disease destroys the cells that produce the hormone, which is crucial to keeping blood sugar in check. But now research suggests a new therapy could finally allow people with type 1 diabetes to make insulin on their own.
A 42-year-old man who has lived most of his life with type 1 diabetes has become the first human to receive a transplant of genetically modified insulin-producing cells that can slip past the immune system’s mistaken attacks. This marks the first pancreatic cell transplant in a human to sidestep the need for immunosuppressant drugs—and it might even lead to a future cure for the disease, researchers say.
“This is the most exciting moment of my scientific career,” says cell biologist Per-Ola Carlsson of Uppsala University in Sweden, who helped develop the procedure. The new treatment, he says, “opens the future possibility of treating not only diabetes but other autoimmune diseases.”
On supporting science journalism
If you’re enjoying this article, consider supporting our award-winning journalism by subscribing. By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
Scientists injected nearly 80 million genetically tweaked cells into the participant’s forearm muscle, and 12 weeks later the cells were still alive and producing insulin. The recipient did require additional insulin injections—but the injected cells showed no signs of rejection, which the researchers say is a major step forward. The results were reported this month in the New England Journal of Medicine.
About two million people in the U.S. live with type 1 diabetes, which typically requires an intensive regimen of insulin injections and blood sugar monitoring. If their blood sugar runs amok, people face severe risks, including heart attacks, nerve damage, vision problems, kidney disease, and more.
For decades, scientists have struggled to develop therapies that can successfully replenish beta cells—the specialized insulin-producing cells that are found in the pancreas. Newly added functional beta cells are usually quickly destroyed because a type 1 diabetic immune system flags them as invaders. A few past attempts successfully transplanted donor islets—clusters of pancreatic cells that included beta cells—but these always ultimately triggered an aggressive immune response. And such a response requires recipients to take lifelong immunosuppressive drugs, which come with serious side effects, such as increased risks of infections and cancer. For example, at a conference in June, Boston-based Vertex Pharmaceuticals announced that 10 out of 12 participants who were treated with a stem-cell-based infusion during a clinical trial no longer required insulin injections a year after the therapy. But they may continue to need to immunosuppressants.
In the new study, Carlsson and his team looked for ways to dodge the immune response. First, they broke down a deceased donor’s pancreatic islets into single cells. Using the common gene-editing technique CRISPR, the researchers inactivated in some of these cells two genes that control the expression of proteins called human leukocyte antigens, which direct the immune system to the foreign cells. Without those markers, the immune system can’t easily recognize and destroy the donor cells.
To further evade immune system detection, the team made some cells express higher levels of a gene that discourages attacks by the body’s natural killer cells and macrophages, two types of immune cells. Three months after the treatment, although the immune system attacked some cells in the graft, it left the cells that had the inactivated genes and overexpressed gene alone. Blood tests showed no measurable immune cell activation or antibody production in response to these cells.
Before the transplant, the participant had no measurable naturally produced insulin and was receiving daily doses of the hormone. But within four to 12 weeks following the transplant, his levels rose slightly on their own after meals—showing that the new beta cells were releasing some insulin in response to glucose. Four adverse events occurred, but none were serious or related to the modified cells.
The advance “is amazing,” says Laura Alonso, chief of the division of endocrinology, diabetes and metabolism at Weill Cornell Medicine, who was not involved in the new study. Unlike type 2 diabetes, in which people have poorly functioning beta cells, type 1 diabetes can destroy beta cells completely. Some people with type 1 diabetes may still have a small set of functional beta cells, but in more established cases, the immune system often whittles away all cells, Alonso says. For those established cases, she says, “cell-based therapy is where we need to go.”
Alonso adds, however, that even though the new study is promising, it involved just one participant and is therefore preliminary. And longer-term monitoring is needed to confirm the therapy’s safety before it can be offered to more people. She also notes that the injected cells produced only 7 percent of the insulin needed for a person to be fully independent of additional medication. The researchers supplied the recipient with insulin doses to maintain healthy blood sugar levels.
“It’s a relatively short but nonetheless important finding,” says Kevan Herold, an endocrinologist at the Yale School of Medicine, who was also not involved in the study. Because the participant still required a substantial amount of insulin after the transplant and no others have received this treatment yet, Harold cautions that “the clinical significance is somewhat unproven.”
Carlsson says the team will continue to monitor the transplant recipient over the next year and will increase the dose of the modified cells if no adverse effects occur. In the meantime, he and his colleagues are developing a stem cell source that would be capable of producing large quantities of insulin-producing cells. “The combination of those two advances would create the possibility of a cure for type 1 diabetes,” he says.
While Herold thinks it’s still too early to consider this approach for a cure, “these options are now here to change the disease in ways that have never been possible before,” he says. “There’s tremendous hope.”