This article is part of “Innovations In: RSV,” an editorially independent special report that was produced with financial support from MSD, Sanofi and AstraZeneca.
When Laura Ehrlich gave birth to her first child in 2020, the COVID-causing virus wasn’t the only threat facing her son. Born a micro preemie at under 26 weeks, little Alistair was also at very high risk for severe disease from other germs, including respiratory syncytial virus (RSV).
Ehrlich says she was “terrified because it was a guaranteed hospital stay for him,” and after he had already spent his first 134 days of life in a neonatal intensive care unit (ICU), “I didn’t want that for him anymore.”
On supporting science journalism
If you’re enjoying this article, consider supporting our award-winning journalism by subscribing. By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
Fortunately, a monoclonal antibody—a protein that mimics the antibodies a person’s immune system would make if they were infected with a particular pathogen—was available. Receiving a monthly dose of palivizumab would substantially reduce the risk that her son would develop a severe case of RSV, should he be exposed to the virus.
Even though Ehrlich had to bring her son in for a shot for each of the approximately five months of a typical RSV season, it was worth the effort.
“It was definitely reassuring to have that extra layer of protection for him,” she says. “I mean, here’s this little baby who was so fragile, and we were 100 percent behind doing everything we could to protect him, including the RSV antibodies.”
When palivizumab received U.S. Food and Drug Administration approval in 1998, it was a lifesaver for fragile infants like Alistair, halving the risk of hospitalization from RSV for these children. But its expense and monthly frequency meant it wasn’t a viable option for the nearly four million babies born each year who weren’t considered to be at high risk but whose developing lungs and immune system still made them vulnerable to serious complications from the virus.
“The majority of babies who [need] to get intubated in the ICU are otherwise healthy babies with no underlying health conditions,” says Jason Terk, a general pediatrician in Keller, Tex., and former president of the Texas Pediatric Society. “It doesn’t kill a whole lot of babies, but it definitely causes a high level of morbidity.”
It wasn’t until the development of Sanofi and AstraZeneca’s nirsevimab, a single-dose monoclonal antibody approved by the FDA in 2023 to help prevent severe RSV in all infants, that a population-level strategy for reducing RSV became available. Nirsevimab provides passive immunity against RSV—giving babies antibodies to fight the virus that their immune systems could not make on their own without an effective vaccine. It’s 76 to 85 percent effective against severe RSV infections and 74 to 90 percent effective against RSV-related hospitalization. The options expanded further this past June with the approval of another single-dose monoclonal antibody, Merck’s clesrovimab, which is 92 percent effective against severe RSV in infants and 84 percent effective against RSV-related hospitalization.
“There are certain inflection points, in my experience, where I can say these were game-changing events,” Terk says. The first was the introduction of a vaccine against Haemophilus influenzae type b (Hib), a bacterium that can cause meningitis. The second was development of a vaccine against rotavirus, a pathogen that causes diarrheal illness. Now the development of these monoclonal antibodies “is the third significant inflection point event,” he says.
RSV is the number one cause of hospitalization among infants, and “you’re talking about an intervention that is going to prevent the majority of hospitalizations that we’ve always seen with RSV,” Terk says.
A Tricky Virus
Scientists tried to develop a vaccine against RSV in the 1960s, after its discovery in 1956. But a disastrous lack of understanding about the virus’s behavior when it fuses with cells meant trials ended in tragedy: Among children who became infected with RSV, the rate of severe disease was more than seven times higher for children who received this vaccine than it was for those who did not. And in one trial, two vaccinated children died from severe RSV they caught in the community.
It would take decades to discover what went wrong: a phenomenon called antibody-dependent enhancement, in which the antibodies the vaccine induced the immune system to make did not effectively neutralize the virus. Instead they worsened the disease.
So scientists turned to a different strategy for protection: passive immunity with monoclonal antibodies. Rather than using active immunity—where a person’s body produces the antibodies themselves—people would receive an injection of the antibodies to battle the virus.
Palivizumab delivered that protection starting in 1998—but at a steep financial and logistical cost.
The list price of palivizumab, before insurance kicks in, is roughly $1,800 per monthly dose. It’s also dosed by a baby’s weight, so larger, full-term infants could require multiple injections. Given these challenges, the FDA recommended palivizumab for limited populations: premature infants born at under 29 weeks old or with chronic lung disease, immunocompromised infants and those with congenital heart disease, Down syndrome, cystic fibrosis, or certain other lung or neuromuscular disorders.
Even then, it was only about 58 percent effective at preventing hospitalization among those vulnerable babies.
At the same time, RSV continued to wreak havoc on other children, hospitalizing about 2 to 3 percent of all babies under one year old from approximately November to March each year, according to James Campbell, an infectious disease pediatrician at the University of Maryland School of Medicine in Baltimore. Infants under six months old who catch RSV are at increased risk of developing viral pneumonitis, where fluid enters lung air spaces and interferes with the exchange of gases, potentially requiring substantial respiratory support, such as supplemental oxygen or a ventilator, Terk says. In addition to causing breathing difficulties, severe RSV increases the risk of a secondary bacterial infection, Campbell adds.
Every season “was an annual heartache,” Terk says. “It was always not whether we were going to have RSV but how bad a season it was going to be.”
Any time a baby arrived with probable RSV, “you just had to kind of prepare families for something that was going to be a tough, tough slog and going to last longer than the typical upper respiratory infection,” he says. “That’s been the reality for the vast majority of my career.”
What families needed was a more effective, less expensive and longer-lasting antibody for all infants.
A process called “reverse vaccinology” opened the door to that antibody and led to the development of immunizations for infants—as well as vaccines for pregnant people and older adults.
Most vaccines are developed by starting with a dead, inactivated, or weakened pathogen or segments of it. Then that pathogen is introduced into the body, causing the immune system to produce antibodies against it. But with reverse vaccinology, scientists start instead with the antibodies and try to determine which ones are most powerful at attacking the pathogen.
To find those powerful antibodies, scientists sort through B cells, a type of white blood cell that makes millions of different antibodies against a particular pathogen. Their goal is to identify the “best-in-class” antibodies that bind to the virus and hinder its entry into the cell, explains Jason McLellan, a molecular biologist at the University of Texas at Austin, whose work led to the development of effective RSV vaccines.
Once researchers study the chosen antibodies’ structure, they can design a vaccine to re-create or manufacture those particular antibodies as a monoclonal antibody treatment, such as nirsevimab.
To develop a monoclonal antibody treatment, the first step is to find those “best-in-class antibodies.” For RSV, that breakthrough came from the blood of a Dutch adult who had likely recently encountered the virus.
Seeking the “Best in Class”
In 2006 a team led by immunologist Hergen Spits at the University of Amsterdam procured blood samples from a local blood bank to screen for antibody effectiveness against RSV.
They had to ensure the B cells in the screened blood lasted long enough to be tested against the virus. Once B cells identify their target pathogen, they multiply and then differentiate into plasma cells, the form of these white blood cells that makes and releases antibodies. The problem for researchers like Spits is that plasma cells burn so much energy to produce antibodies that they become spent and unable to reproduce, he explains.
So his team introduced a couple of genes from cancer cells into the B cells circulating in screened blood. This trick stopped the B cells from completing their normal transition into antibody-producing plasma cells, when they normally cease dividing. Instead the modified cells kept multiplying indefinitely while also secreting lots of antibodies.
At that point, most researchers would first test for antibodies that attached to the virus before testing for those that neutralized the pathogen. But crucially, Spits’s team flipped that script.
“The most important decision we made [was] to screen for neutralization,” Spits says.
Once the researchers had antibodies that neutralized the live virus, however, the team tested them on the inactivated virus and discovered they would not bind to it. Spits and his colleagues concluded that the part of the virus that bound with the most effective antibodies only existed on live viruses.
When the team introduced the antibodies to live viruses, it discovered three that neutralized the virus 100 times more efficiently than palivizumab did. The researchers named them D25, AM22 and AM14. Finally, scientists had unlocked the code to allow them to begin developing a highly potent monoclonal antibody.
At that point, Spits passed the baton across the Atlantic. The company MedImmune, based in Gaithersburg, Md., licensed the three antibodies from AIMM, the company that Spits had founded, to overcome the next hurdle: how to increase the half-life of the antibodies so infants could receive only one injection.
To develop a marketable product, MedImmune’s team needed to “get a potent enough molecule and increase the half-life to the point where a maximum dose was sufficient to protect all infants,” says JoAnn Suzich, one of the lead scientists who worked on nirsevimab.
MedImmune, which by then had been acquired by AstraZeneca, had already been working on a way to extend the half-life and eventually found one. By swapping out a handful of amino acids at the base of the antibody stem—called the YTE mutation—the researchers extended the half-life from approximately 20 days for palivizumab to around 70 days for the D25 antibody. The newly modified antibody, now christened MEDI8897, was on its way to becoming nirsevimab.
The Home Stretch
Around the same time, McLellan and a team of scientists at the nearby National Institute of Allergy and Infectious Diseases were working to unlock another mystery critical to the creation of an effective vaccine: Why would some antibodies bind to RSV but fail to neutralize it?
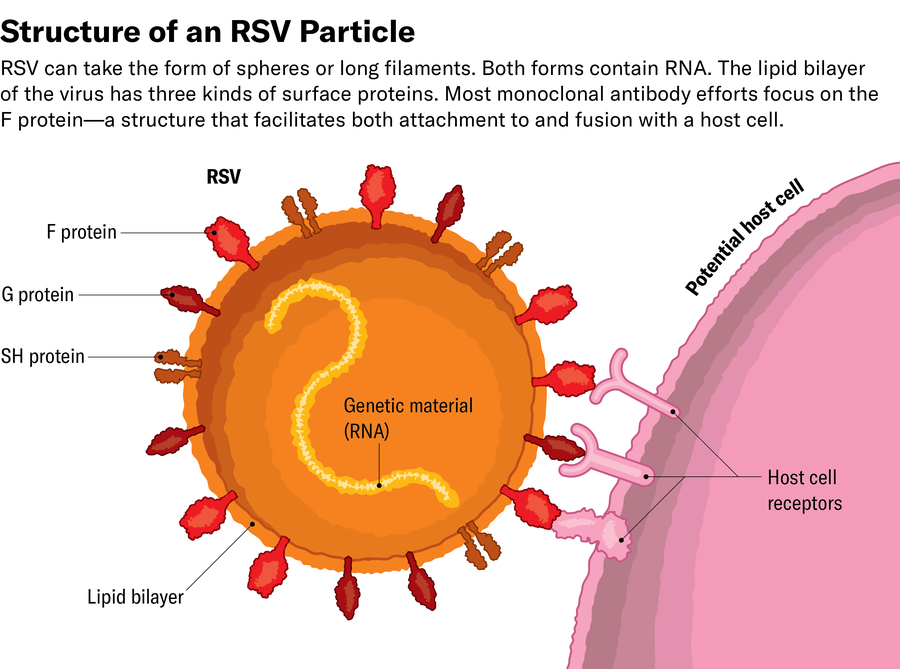
The secret involved one of RSV’s surface proteins, the F protein, which allows the virus to fuse its viral membrane with the cell membrane. Once bound, the virus can inject its genetic material (RNA in this case) into the cell, which is then transformed into a viral-making machine.
Using x-ray crystallography and, later, cryo-electron microscopy, McLellan studied the structure of the F protein and discovered that it changes shape after fusing with the cell. In mapping the structure of the F protein, both before and after fusion, McLellan’s team concluded that antibodies that bound to the postfusion protein did not neutralize the virus. Because the tragic 1960s trial used an inactivated vaccine—which only contained postfusion RSV—the antibodies it produced were toothless against the virus before it attached to cells. This also explained why Spits’s neutralizing antibodies would not bind to the inactivated virus.

Jen Christiansen; Sources: Reference illustration by Haye Nijhuis and Tim Beaumont, Amsterdam University Medical Center (protein forms); Hergen Spits (expert reviewer)
After solving this final piece of the puzzle, McLellan’s team developed a way to “staple” the prefusion F protein in place, stabilizing it and ultimately leading to the development of an effective RSV vaccine.
McLellan’s work also helped elucidate why D25 was so much more potent than palivizumab at preventing infection. Palivizumab bound to the prefusion and postfusion F proteins, but the most strongly neutralizing antibodies against RSV were those that only targeted the virus’s prefusion structure.
At last, 17 years after Spits had begun the search for a potent antibody against RSV, his discovery had led scientists to better understand the virus and to create multiple ways of preventing severe disease from it. By the end of the summer of 2023, just in time for the fall RSV season, the FDA had approved one preventive monoclonal antibody and two vaccines against RSV.
GlaxoSmithKline’s Arexvy vaccine and Pfizer’s Abrysvo vaccine both protect older adults. And Abrysvo can also be given during pregnancy to stimulate the production of antibodies that then pass through the placenta to the fetus and provide a baby with protection after birth.
AstraZeneca partnered with Sanofi to make and market the highly effective monoclonal antibody nirsevimab for all infants. In its phase 3 clinical trial, nirsevimab was 75 percent effective against RSV that required any kind of medical attention and 62 percent effective against RSV-related hospitalization. In a larger trial published five months after the drug’s approval, nirsevimab was 83 percent effective against RSV-related hospitalization.
But like any virus, RSV has the ability to mutate, so at least one question remained: Could the virus eventually outwit nirsevimab?
“You can imagine that if you use one monoclonal antibody for the whole population, then particular variants of the virus can pop up which cannot be neutralized by the antibody,” Spits says.
A study by researchers in France determined that a mutant RSV strain could develop resistance to nirsevimab but only rarely. Minimizing this risk became one of the scientists’ key primary goals while developing clesrovimab, the monoclonal antibody that received FDA approval in June, says Tarit Mukhopadhyay, head of infectious disease and vaccine discovery at Merck. The team specifically sought an antibody that would bind to an essential part of the virus; that way, the virus could not afford to mutate in a way that deleted or modified that spot, he says.
The researchers also prioritized an extended half-life—just as MedImmune did—as well as formulating the antibody to fit into a single prefilled syringe that did not depend on a child’s weight. Nirsevimab comes in two different dosages for infants younger than eight months, depending on whether they weigh under five kilograms or five kilograms and above.
Clesrovimab meets all those criteria: its half-life is long enough to last a full RSV season, and, unlike nirsevimab, it can be given to any infant of any weight. It also binds to a part of the prefusion F protein that remains conserved even when the virus mutates. If the virus mutates to dispense with the site clesrovimab binds to, it becomes less able to infect cells.
“The risk of creating resistant mutants to clesrovimab is going to be super low,” Mukhopadhyay says.
“Turning Point”
Today, nearly three decades after palivizumab provided a way to protect the most vulnerable infants from RSV, families have three options for protecting any baby from severe disease: the maternal vaccine given during pregnancy and two monoclonal antibodies, nirsevimab and clesrovimab, administered after birth.
“I think we are at a turning point in antibody treatments and how we think about them,” Mukhopadhyay says. In the past, antibody treatments were typically intravenous infusions delivered over hours with frequent dosing and worries about viral escape, he says. “The easier we can make it to use these medicines and reduce barriers to implementation means that more lives are protected,” Mukhopadhyay adds, “and that’s really what this is all about.”
Ehrlich, whose son spent 134 days in a hospital because of his premature birth, says it’s wonderful that parents now have the chance to reduce the risk for all babies. “I think that if you have an option to protect your child, you have an obligation to do so,” Ehrlich says.
Another parent who’s grateful for nirsevimab is Suzich, who worked on its development at MedImmune. Her first grandchild, born two weeks before she spoke with Scientific American, had just received nirsevimab. “I was walking around holding her yesterday, saying, ‘You know what? Your grandmother developed that,’” Suzich says. “She didn’t seem to be interested, but that’s okay.”

