Pierson, T. C. & Diamond, M. S. The continued threat of emerging flaviviruses. Nat. Microbiol. 5, 796–812 (2020).
Fishburn, A. T., Pham, O. H., Kenaston, M. W., Beesabathuni, N. S. & Shah, P. S. Let’s get physical: flavivirus-host protein-protein interactions in replication and pathogenesis. Front. Microbiol. 13, 847588 (2022).
Anwar, M. N. et al. The interactions of flaviviruses with cellular receptors: Implications for virus entry. Virology 568, 77–85 (2022).
Pan, Y. et al. Flaviviruses: innate immunity, inflammasome activation, inflammatory cell death, and cytokines. Front. Immunol. 13, 829433 (2022).
Lopes, R. L. et al. Kidney involvement in yellow fever: a review. Rev. Inst. Med. Trop. Sao Paulo 61, e35 (2019).
Monath, T. P. & Vasconcelos, P. F. Yellow fever. J. Clin. Virol. 64, 160–173 (2015).
Collins, N. D. & Barrett, A. D. Live attenuated yellow fever 17D vaccine: a legacy vaccine still controlling outbreaks in modern day. Curr. Infect. Dis. Rep. 19, 14 (2017).
Gianchecchi, E., Cianchi, V., Torelli, A. & Montomoli, E. Yellow fever-origin, epidemiology, preventive strategies and future prospects. Vaccines 10, 372 (2022).
Zimmerman, O., Holmes, A. C., Kafai, N. M., Adams, L. J. & Diamond, M. S. Entry receptors—the gateway to alphavirus infection. J. Clin. Invest. 133, e165307 (2023).
Hastings, A. K. et al. TAM receptors are not required for Zika virus infection in mice. Cell Rep. 19, 558–568 (2017).
Laureti, M., Narayanan, D., Rodriguez-Andres, J., Fazakerley, J. K. & Kedzierski, L. Flavivirus receptors: diversity, identity, and cell entry. Front. Immunol. 9, 2180 (2018).
Alen, M. M., Dallmeier, K., Balzarini, J., Neyts, J. & Schols, D. Crucial role of the N-glycans on the viral E-envelope glycoprotein in DC-SIGN-mediated dengue virus infection. Antiviral Res. 96, 280–287 (2012).
Perera-Lecoin, M., Meertens, L., Carnec, X. & Amara, A. Flavivirus entry receptors: an update. Viruses 6, 69–88 (2013).
Carnec, X. et al. The phosphatidylserine and phosphatidylethanolamine receptor CD300a binds Dengue virus and enhances infection. J. Virol. 90, 92–102 (2016).
Cordero-Rivera, C. D. et al. The importance of viral and cellular factors on flavivirus entry. Curr. Opin. Virol. 49, 164–175 (2021).
Lee, E. & Lobigs, M. E protein domain III determinants of yellow fever virus 17D vaccine strain enhance binding to glycosaminoglycans, impede virus spread, and attenuate virulence. J. Virol. 82, 6024–6033 (2008).
Nahain, A. A. et al. Antiviral activities of heparan sulfate mimetic RAFT polymers against mosquito-borne viruses. ACS Appl. Bio Mater. 7, 2862–2871 (2024).
Pönighaus, C. et al. Human xylosyltransferase II is involved in the biosynthesis of the uniform tetrasaccharide linkage region in chondroitin sulfate and heparan sulfate proteoglycans. J. Biol. Chem. 282, 5201–5206 (2007).
DePew, A. T. & Mosca, T. J. Conservation and innovation: versatile roles for LRP4 in nervous system development. J. Dev. Biol. 9, 9 (2021).
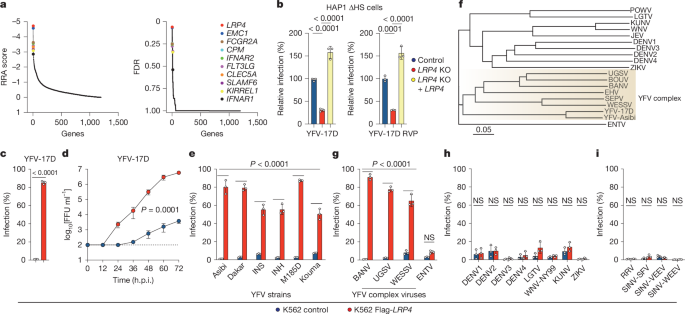
Hoffmann, H. H. et al. TMEM41B is a pan-flavivirus host factor. Cell 184, 133–148 (2021).
Lin, D. L. et al. The ER membrane protein complex promotes biogenesis of Dengue and Zika virus non-structural multi-pass transmembrane proteins to support infection. Cell Rep. 27, 1666–1674 (2019).
Marceau, C. D. et al. Genetic dissection of Flaviviridae host factors through genome-scale CRISPR screens. Nature 535, 159–163 (2016).
Ma, H. et al. A CRISPR-based screen identifies genes essential for West-Nile-virus-induced cell death. Cell Rep. 12, 673–683 (2015).
Khandia, R. et al. Modulation of Dengue/Zika virus pathogenicity by antibody-dependent enhancement and strategies to protect against enhancement in Zika virus infection. Front. Immunol. 9, 597 (2018).
Santos-Peral, A. et al. Prior flavivirus immunity skews the yellow fever vaccine response to cross-reactive antibodies with potential to enhance dengue virus infection. Nat. Commun. 15, 1696 (2024).
Qiu, X. & Bailey, A. L. Two mutations in NS2B are responsible for attenuation of the yellow fever virus (YFV) vaccine strain 17D. PLoS Pathog. 21, e1013373 (2025).
Zhang, J. et al. Amino acid changes in two viral proteins drive attenuation of the yellow fever 17D vaccine. Nat. Microbiol. 10, 1902–1917 (2025).
Abdullahi, I. N. et al. The interplay between environmental factors, vector competence and vaccine immunodynamics as possible explanation of the 2019 yellow fever re-emergence in Nigeria. N. Microbes N. Infect. 41, 100858 (2021).
Hobson-Peters, J. et al. A recombinant platform for flavivirus vaccines and diagnostics using chimeras of a new insect-specific virus. Sci. Transl. Med. 11, eaax7888 (2019).
Hardy, J. M. et al. A unified route for flavivirus structures uncovers essential pocket factors conserved across pathogenic viruses. Nat. Commun. 12, 3266 (2021).
Rey, F. A., Heinz, F. X., Mandl, C., Kunz, C. & Harrison, S. C. The envelope glycoprotein from tick-borne encephalitis virus at 2 A resolution. Nature 375, 291–298 (1995).
Volk, D. E. et al. Solution structure and antibody binding studies of the envelope protein domain III from the New York strain of West Nile virus. J. Biol. Chem. 279, 38755–38761 (2004).
Cao, D., Ma, B., Cao, Z., Zhang, X. & Xiang, Y. Structure of Semliki Forest virus in complex with its receptor VLDLR. Cell 186, 2208–2218 (2023).
Adams, L. J. et al. Structural and functional basis of VLDLR usage by Eastern equine encephalitis virus. Cell 187, 360–374 (2024).
Davis, C. W. et al. West Nile virus discriminates between DC-SIGN and DC-SIGNR for cellular attachment and infection. J. Virol. 80, 1290–1301 (2006).
Monath, T. P. & Barrett, A. D. Pathogenesis and pathophysiology of yellow fever. Adv. Virus Res. 60, 343–395 (2003).
Bailey, A. L. et al. Consumptive coagulopathy of severe yellow fever occurs independently of hepatocellular tropism and massive hepatic injury. Proc. Natl Acad. Sci. USA 117, 32648–32656 (2020).
Meier, K. C., Gardner, C. L., Khoretonenko, M. V., Klimstra, W. B. & Ryman, K. D. A mouse model for studying viscerotropic disease caused by yellow fever virus infection. PLoS Pathog. 5, e1000614 (2009).
Kafai, N. M. et al. Entry receptor LDLRAD3 is required for Venezuelan equine encephalitis virus peripheral infection and neurotropism leading to pathogenesis in mice. Cell Rep. 42, 112946 (2023).
Ma, H. et al. LDLRAD3 is a receptor for Venezuelan equine encephalitis virus. Nature 588, 308–314 (2020).
Johnson, E. B., Hammer, R. E. & Herz, J. Abnormal development of the apical ectodermal ridge and polysyndactyly in Megf7-deficient mice. Hum. Mol. Genet. 14, 3523–3538 (2005).
Weatherbee, S. D., Anderson, K. V. & Niswander, L. A. LDL-receptor-related protein 4 is crucial for formation of the neuromuscular junction. Development 133, 4993–5000 (2006).
Bhaskar, M., Satheesan, A. & Basu, A. Low-density lipoprotein receptor is an important host factor in flaviviral entry and replication in neurons. Biochem. Biophys. Res. Commun. 743, 151160 (2024).
Huerta, V. et al. The low-density lipoprotein receptor-related protein-1 is essential for dengue virus infection. Viruses 16, 1692 (2024).
Ganaie, S. S. et al. Lrp1 is a host entry factor for Rift Valley fever virus. Cell 184, 5163–5178 (2021).
Willnow, T. E., Armstrong, S. A., Hammer, R. E. & Herz, J. Functional expression of low density lipoprotein receptor-related protein is controlled by receptor-associated protein in vivo. Proc. Natl Acad. Sci. USA 92, 4537–4541 (1995).
Schwarz, M. M. et al. Oropouche orthobunyavirus infection is mediated by the cellular host factor Lrp1. Proc. Natl Acad. Sci. USA 119, e2204706119 (2022).
Clark, L. E. et al. VLDLR and ApoER2 are receptors for multiple alphaviruses. Nature 602, 475–480 (2022).
Li, W. et al. Shifts in receptors during submergence of an encephalitic arbovirus. Nature 632, 614–621 (2024).
Zhai, X. et al. LDLR is used as a cell entry receptor by multiple alphaviruses. Nat. Commun. 15, 622 (2024).
Palakurty, S. et al. The VLDLR entry receptor is required for the pathogenesis of multiple encephalitic alphaviruses. Cell Rep. 43, 114809 (2024).
Erickson, A. K. & Pfeiffer, J. K. Spectrum of disease outcomes in mice infected with YFV-17D. J. Gen. Virol. 96, 1328–1339 (2015).
Ma, B., Huang, C., Ma, J., Xiang, Y. & Zhang, X. Structure of Venezuelan equine encephalitis virus with its receptor LDLRAD3. Nature 598, 677–681 (2021).
Shen, C., Xiong, W. C. & Mei, L. LRP4 in neuromuscular junction and bone development and diseases. Bone 80, 101–108 (2015).
Davis, C. W. et al. The location of asparagine-linked glycans on West Nile virions controls their interactions with CD209 (dendritic cell-specific ICAM-3 grabbing nonintegrin). J. Biol. Chem. 281, 37183–37194 (2006).
Muller, U. et al. Functional role of type I and type II interferons in antiviral defense. Science264, 1918–1921 (1994).
White, J. P. et al. Intestinal dysmotility syndromes following systemic infection by flaviviruses. Cell 175, 1198–1212 (2018).
Chen, R. E. et al. Implications of a highly divergent dengue virus strain for cross-neutralization, protection, and vaccine immunity. Cell Host Microbe 29, 1634–1648 (2021).
VanBlargan, L. A. et al. Broadly neutralizing monoclonal antibodies protect against multiple tick-borne flaviviruses. J. Exp. Med. 218, e20210174 (2021).
McArthur, M. A., Suderman, M. T., Mutebi, J. P., Xiao, S. Y. & Barrett, A. D. Molecular characterization of a hamster viscerotropic strain of yellow fever virus. J. Virol. 77, 1462–1468 (2003).
Goo, L., VanBlargan, L. A., Dowd, K. A., Diamond, M. S. & Pierson, T. C. A single mutation in the envelope protein modulates flavivirus antigenicity, stability, and pathogenesis. PLoS Pathog. 13, e1006178 (2017).
Sievers, F. et al. Fast, scalable generation of high-quality protein multiple sequence alignments using Clustal Omega. Mol. Syst. Biol. 7, 539 (2011).
Yu, G. C., Smith, D. K., Zhu, H. C., Guan, Y. & Lam, T. T. Y. GGTREE: an R package for visualization and annotation of phylogenetic trees with their covariates and other associated data. Methods Ecol. Evol. 8, 28–36 (2017).
Bodenhofer, U., Bonatesta, E., Horejs-Kainrath, C. & Hochreiter, S. msa: an R package for multiple sequence alignment. Bioinformatics 31, 3997–3999 (2015).
Sanson, K. R. et al. Optimized libraries for CRISPR-Cas9 genetic screens with multiple modalities. Nat. Commun. 9, 5416 (2018).
Li, W. et al. MAGeCK enables robust identification of essential genes from genome-scale CRISPR/Cas9 knockout screens. Genome Biol. 15, 554 (2014).
Miyoshi, H. & Stappenbeck, T. S. In vitro expansion and genetic modification of gastrointestinal stem cells in spheroid culture. Nat. Protoc. 8, 2471–2482 (2013).
Huch, M. et al. Long-term culture of genome-stable bipotent stem cells from adult human liver. Cell 160, 299–312 (2015).
Huch, M. et al. In vitro expansion of single Lgr5+ liver stem cells induced by Wnt-driven regeneration. Nature 494, 247–250 (2013).
Doyle, M. P. et al. Isolation of a potently neutralizing and protective human monoclonal antibody targeting yellow fever virus. mBio 13, e0051222 (2022).
Kim, A. S. et al. Pan-protective anti-alphavirus human antibodies target a conserved E1 protein epitope. Cell 184, 4414–4429 (2021).
Nelson, C. A., Lee, C. A. & Fremont, D. H. Oxidative refolding from inclusion bodies. Methods Mol. Biol. 1140, 145–157 (2014).
Oliphant, T. et al. Antibody recognition and neutralization determinants on domains I and II of West Nile Virus envelope protein. J. Virol. 80, 12149–12159 (2006).
BIAevaluation Version 3.0 Software Handbook (Biacore AB, 1997).